Have you recently had or are scheduled for surgery in or around your pelvis?
Pelvic surgery refers to any surgery done in the pelvic area, including the following:
- Prolapse repair (this includes both anterior, posterior and apical vaginal wall prolapse)
- Prostate surgery
- Radical prostatectomy
- Transurethral Resection of the Prostate (TURP)
- Inguinal hernia repair
- Hysterectomy
- Oophorectomy/salpingectomy (ovaries and/or fallopian tube removal)
- Endometriosis surgery (this includes a laparoscopic surgery)
- Gender affirming surgeries
- Surgery following pelvic cancers (this includes uterine, cervical, endometrial, bowel, rectal, bladder and many others!)
- Surgeries for stress incontinence (bladder leakage)
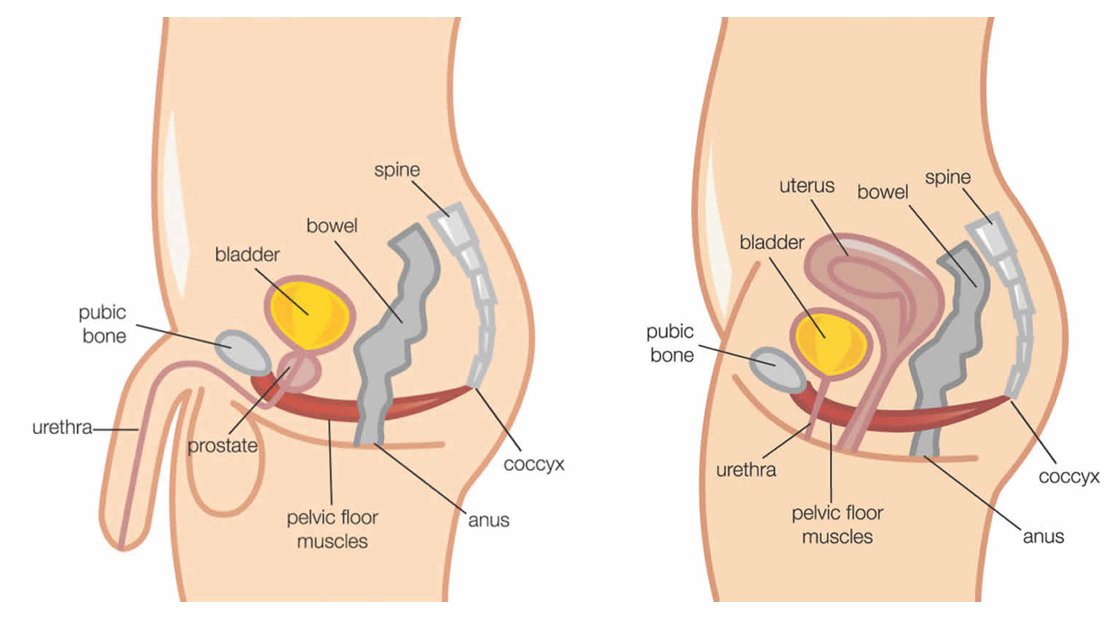
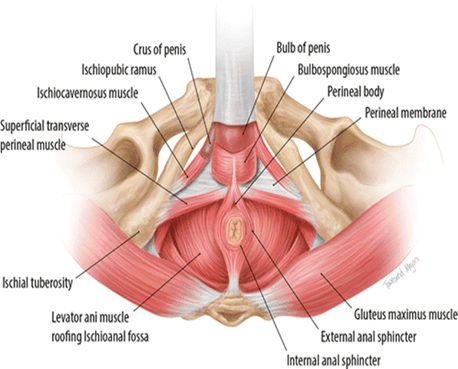
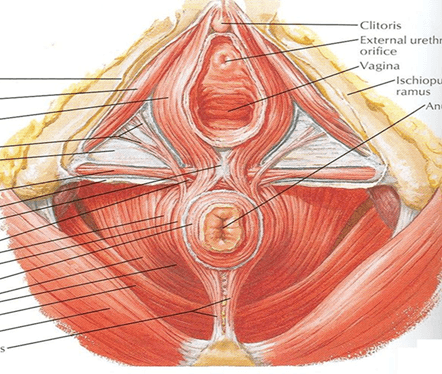
What is the Pelvic Floor?
The pelvic floor is a large group of muscles that run from the pubic bone to the anus and span laterally from hip to hip. The pelvic floor muscles have the following functions:
- Support – these muscles help support our organs against the effects of gravity and increases in intra-abdominal pressure
- Sphincteric – provides us with faecal and urinary continence
- Sump-Pump – acts like a sump pump for our venous and lymphatic systems
- Sexual – responsible for orgasm and sensations related to sexual function
- Stability – provides stability to the pelvic, lumbo-pelvic and hip joints
The pelvic floor muscles are often involved during many pelvic surgeries. Some surgeries make small incisions into the body, whereas other surgeries may involve a larger area of tissue or the implantation of foreign bodies.
Why Go to Physiotherapy?
Physiotherapy can help with many different aspects of surgery, both before and after. Many times the surgery is working on the organs and tissues within the pelvis, but what about the muscles within that area? The muscles inside of our pelvis are not commonly ones that we are familiar with. Nobody teaches us! It is important to know how to locate these muscles, understand their importance to the pelvis and the rest of the body, and learn how to train them. This can often require a specially-trained Physiotherapist to assess and treat this area.
Do you know many of us do not properly activate our pelvic floor muscles (also referred to as a “kegel”) in the correct way! Training the pelvic floor is not a one size fits all exercise and everyone requires an individualised treatment plan according to the assessment findings and surgery that has occurred. Training these muscles appropriately can be really helpful for a successful surgical outcome long term.
What to Expect?
Pelvic surgery can be separated into three different phases:
- Pre-surgery: getting you prepared for surgery
- Post-surgical rehabilitation: focuses on regaining strength, tissue range of motion, motor control, and endurance
- Return to activity: allowing you to get back to the activities you enjoy!
Pre-surgery
It is always recommended to come in for an appointment prior to having a pelvic surgery. This phase helps you get ready for the surgery by ensuring you have the skills and tools necessary for both the surgery and the early days post op (including activities of daily living at home and toileting after a surgery).

Post-surgical Rehabilitation
We will follow up with you after your surgery to help guide you from the early days of release from hospital to being able to get back to activities and exercise. The goal of this phase is to load the tissue surrounding the surgical area and get you back to movement. This can include anything from ensuring healthy bladder routines and bowel movements, returning to sexual intercourse and getting you back to activities of daily life.
During this phase your Physiotherapist will guide you through tissue healing, scar mobility work (if appropriate), increased range of motion and gradual loading of the tissue.
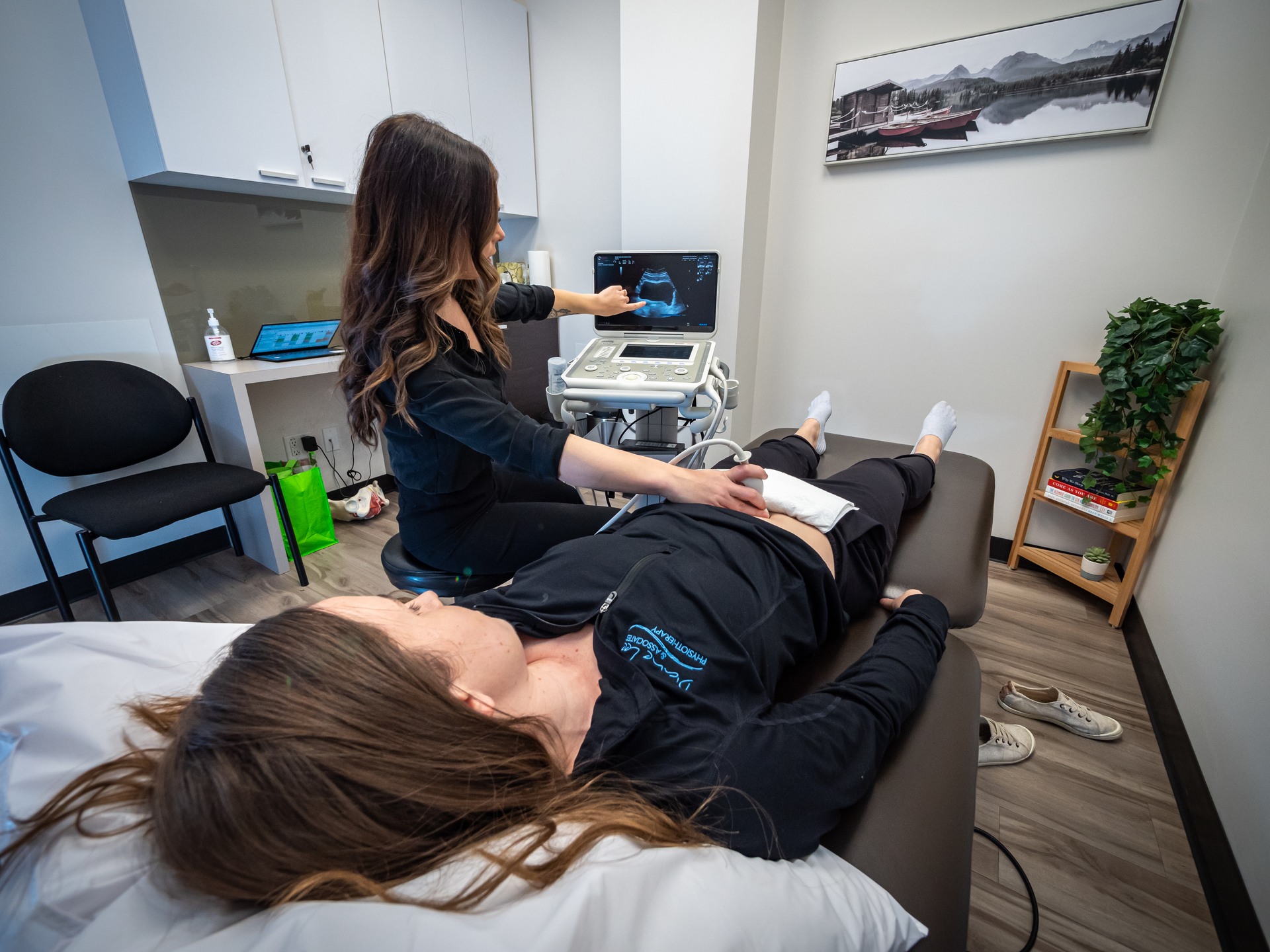
Assessment and treatment at Diane Lee & Associates may include an internal examination (vaginal and/or anal), the use of real time ultrasound to be able to assess the mobility and function of the tissue, manual therapy, dry needling, visceral manipulation, motor control training (waking up inhibited muscles and reducing bracing strategies) and exercise prescription.
Return to Activity
As you continue to progress through your treatment plan it is important to get you back to the activities that you enjoy! This can be workouts at the gym, participation in sports or running around in the yard with your kids. It’s all up to you!

We look forward to working with you!




