Spinal surgery may be part of your journey to recovery if you have:
- An age related degenerative spine condition that is impacting the nerves
- Experienced trauma to the spine involving its bony components and stabilization is required
- A condition which results in complex spinal deformity
Physiotherapy while you are preparing for spinal surgery
Pre-operative physiotherapy helps to prepare you for surgery. The stronger you are, the easier your recovery will be. The goal of these sessions are:

- to help you restore muscle strength while waiting for the surgery and
- to learn exercises to prepare for the rehabilitation process. These exercises may include those to:
- improve breathing function,
- optimize your core trunk muscles (your diaphragm, pelvic floor, abdominal and spine muscles).
- Improve the strength of your arms and legs.
It is a great opportunity to learn exercises ahead of time and practice how you will move in and out of bed, or walk with a walker etc.
Physiotherapy after spinal surgery
- Recovering in the early days: Whether you are recovering at the hospital or at home, it is important to maintain safe and optimal movement of your entire body. Physiotherapy can help you with mobility with exercises that focus on other parts of your body (hips, knees, shoulders, neck). You will also be taught various ways of getting in and out of bed, or rolling over. You will also learn how to monitor and treat your surgical scar. Your surgeon will provide a limit to certain activities or loads, and these will be followed closely. The goal of this phase is for you to safely return to your activities of daily living (self-care and ambulation at home).
- Rehabilitation in the first weeks and months: This phase follows after you have regained some, or most, of your general mobility and strength. Now, physiotherapy will focus on specific areas that you are still struggling with (your goals), such as walking pain free, posture while sitting, balance in standing, optimal scar and soft tissue mobility (think of tight back muscles).
- Return to sport and activities after months and year(s): Certain surgeries require a lengthy rehabilitation process. Eventually your goals will shift to being able to return to sport or activities such as playing golf, hiking, running or biking etc. In this phase, physiotherapy continues to focus on your goals and your program will be individualized and specific to the activity you wish to return to.

Surgery after spinal trauma or cancer
Injury to the spine typically occurs with a sudden traumatic blow in incidents such as car accidents and high impact hits following a fall or a jump.
High-energy blunt trauma to the spinal column may result in vertebral fractures, dislocations, crushes or compression injuries. Please note, that we are not discussing trauma that results in spinal cord injuries here.
Low-energy trauma to the spinal column may result in fractures of the spinal column when there is poor vertebral health (osteoporosis, cancer).
The most common reason we see patients following spinal trauma is:
- Cancer related spinal fracture
- Compression fractures of the thoracic and lumbar spine
- Sport related cervical spine fracture
Cancer related spinal fractures
The bones in the spine can be weakened due to certain types of cancer that can also lead to compression fracture; such as multiple myeloma (the cancer of the bone marrow) or Ewing sarcoma (small round cell sarcoma that forms in the bone). Rehabilitation and cancer can include multiple areas of the body, depending on the type and region of cancer and the treatment you require. To read more about Cancer Rehabilitation at our clinic please visit our Cancer Rehabilitation page.
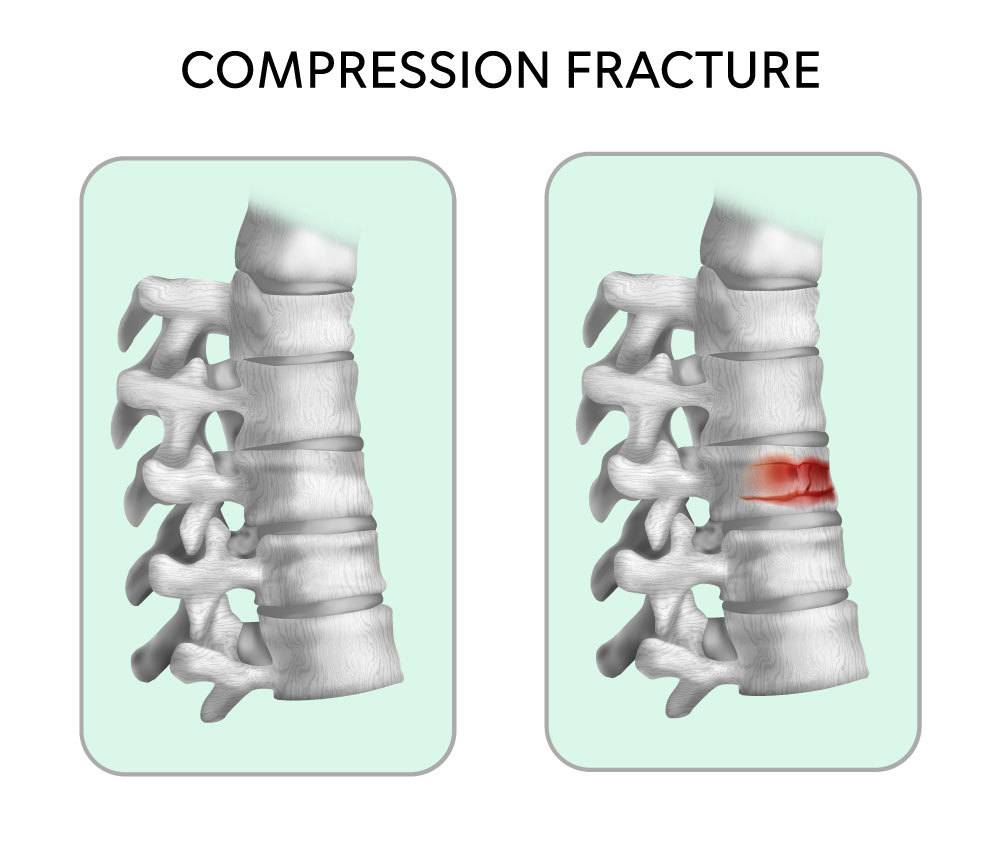
Compression fracture of the thoracic and lumbar spine
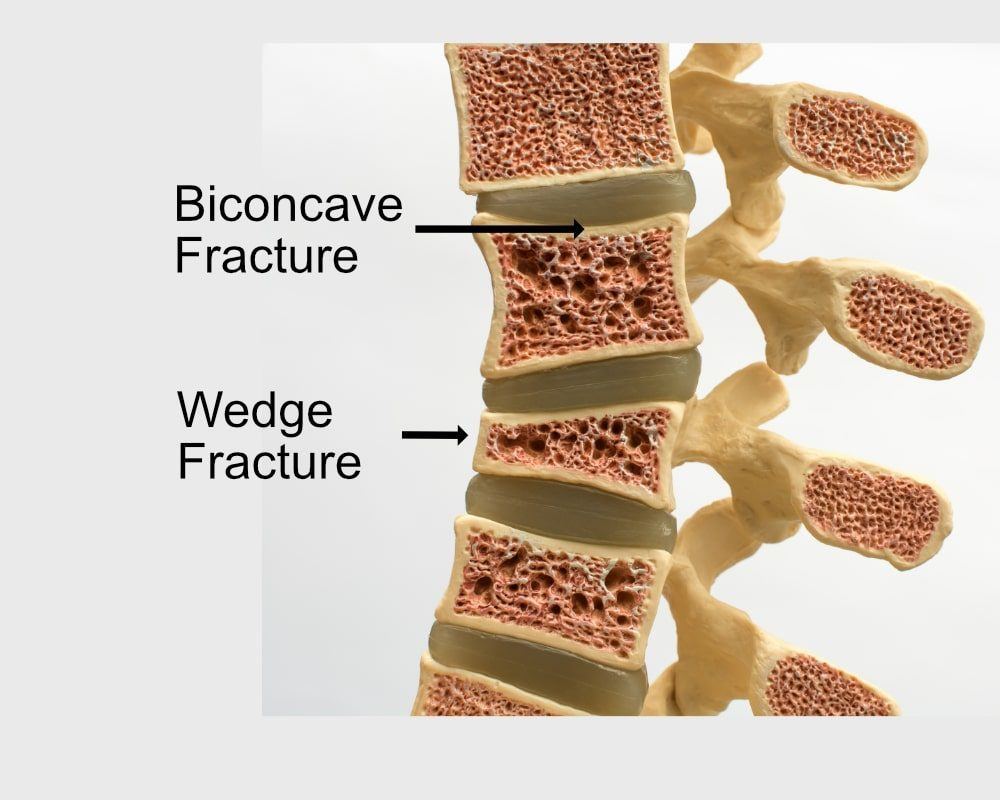
Over 60% of spinal injuries resulting in fracture happen at the thoracolumbar junction (T12-L1); the mechanical transition region between the middle and lower back. The most common type of vertebral compression fracture is a wedge fracture, in which the front of the vertebra breaks, creating a wedge shape. The other type of vertebral compression is the axial burst fracture, in which the vertebra collapses in both the front and back.
Compression fractures can develop due to sudden, high-impact traumas, typically in the younger adult population; and can also develop over time as we age due to osteoporosis or other degenerative spine changes and often activities, such as lifting a heavy object, sneezing, or coughing may cause fractures.
Patients commonly report severe, irritable back pain, reduced physical activity and difficulty with taking a deep breath or finding a comfortable position to rest.
Due to the wedge shaped vertebra the spine now presents more rounded, or ‘kyphotic’, with up to a couple inches of height loss.
Physiotherapy management after compression fracture of the spine
Your rehabilitation following compression vertebral fracture depends on how stable the fracture is. If the bones are considered ‘stable’ and does not require surgical intervention, you can continue your recovery at home and begin conservative management almost immediately. Most patients recover within the first 3 months following the injury.
- Recovering in the early days: Your medical team will provide limits to certain activities or loads, and these will be followed closely. You will also be taught various ways of getting in and out of bed, or rolling over. The goal of this phase is for you to safely return to your activities of daily living (self-care and ambulation at home). Physiotherapy can also help you in the early days and weeks by learning how, and when, to use a support brace and how to manage your pain.

- Rehabilitation in the first weeks and months: This phase follows after you have regained some, or most, of your general mobility and strength. Now, physiotherapy will focus on specific areas that you are still struggling with (your goals), such as walking pain free, posture while sitting, balance in standing, and soft tissue mobility (think of tight back muscles).

- Return to sport and activities after months and year(s): Once the fracture has healed, typically around 12 weeks, an individualized exercise routine will help you support a new posture alignment to develop a dynamic stability above and below the wedge shape vertebra, and to improve muscle balance and breathing function. Some patients require a lengthy rehabilitation process. Eventually your goals will shift to being able to return to sport or activities such as playing golf, hiking, running or biking etc. In this phase, physiotherapy continues to focus on your goals and your program will be individualized and specific to the activity you wish to return to.

Surgical management of compression spinal fracture
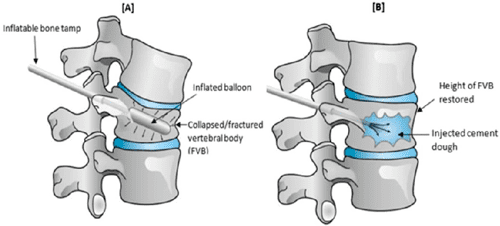
Two common minimal invasive procedures to treat vertebral compression fractures are:
- vertebroplasty and
- kyphoplasty
Both procedures treat the injured vertebra by restoring its height and injecting cement into the fractured vertebra.
Physiotherapy after spinal surgery
Since there are various spinal surgeries, the timeline for each phase of recovery are determined by your surgeon. Commitment to your program, and its timelines, will set you up for the best outcome.
- Recovering in the early days: Whether you are recovering at the hospital or at home, it is important to maintain safe and optimal movement of your entire body. Physiotherapy can help you with mobility with exercises that focus on other parts of your body (hips, knees, shoulders, neck). You will also be taught various ways of getting in and out of bed, or rolling over. You will also learn how to monitor and treat your surgical scar. Your surgeon will provide limits to certain activities or loads, and these will be followed closely. The goal of this phase is for you to safely return to your activities of daily living (self-care and ambulation at home).

- Rehabilitation in the first weeks and months: This phase follows after you have regained some, or most, of your general mobility and strength. Now, physiotherapy will focus on specific areas that you are still struggling with (your goals), such as walking pain free, posture while sitting, balance in standing, optimal scar and soft tissue mobility (think of tight back muscles).
- Return to sport and activities after months and year(s): Certain surgeries require a lengthy rehabilitation process. Eventually your goals will shift to being able to return to sport or activities such as playing golf, hiking, running or biking etc. In this phase, physiotherapy continues to focus on your goals and your program will be individualized and specific to the activity you wish to return to.

Sport related cervical spine fracture
Injuries to the neck can occur in contact sports such as football, soccer, and rugby as well as non-contact sports such as cycling, horseback riding and gymnastics. A fractured vertebra in the cervical spine is more serious and can be life threatening/changing in case of a spinal cord injury, therefore surgical management is more common in this region of the spine.
Injuries to the neck can occur in contact sports such as football, soccer, and rugby as well as non-contact sports such as cycling, horseback riding and gymnastics. A fractured vertebra in the cervical spine is more serious and can be life threatening/changing in case of a spinal cord injury, therefore surgical management is more common in this region of the spine.

Neck injuries can damage multiple anatomical structures including:
- Cervical vertebra fracture and dislocation. A fracture of the cervical vertebra doesn’t always lead to subluxation (shifting) of the bones or injury to the spinal cord or emerging nerves. However, when the ligaments connecting the cervical vertebrae are damaged, shifting, or complete dislocation, of the vertebra can occur and often there are more structures damaged than the cervical vertebrae
- Nerve root(s) or brachial plexus
- Intervertebral disc
Surgery and Rehabilitation for Complex Spinal Deformities
While most structural changes impact one or two segments in the spine; aging, degeneration and increased asymmetric load can lead to complex spinal asymmetries and deformity. This is commonly diagnosed as spondylolisthesis, scoliosis or kyphosis.
These conditions often require more difficult and longer surgical interventions, where more spinal segments, or complete spinal regions including the pelvis, are involved in the procedure.
Some surgeries correct the progression of an idiopathic spinal deformity, a condition that has developed during childhood and progressed further in adulthood. It can be crucial to realign the spine to restore a more optimal posture and balance for optimal function during everyday actives as well as to manage pain. Patients may also need a complex spinal surgery to revise a previous spinal fusion that failed to heal, or to remove hardware following an infection or an accident.

It's never too late to start

Physiotherapy is not just for the immediate rehabilitation phase and the first few months after surgery. Many clients start physiotherapy years, or even decades, after a spinal fusion or Harrington Rod surgery. When combined with scoliosis or kyphosis specific exercises, physiotherapy can be helpful to:
- Improve muscle balance and postural endurance
- Manage pain
- Improve breathing
- Increase overall strength


 Patients with degenerative spine conditions commonly report difficulty with everyday activities, as well as lower back pain and symptoms that radiate or shoot down the leg, such as numbness, tingling, or electric shock like symptoms. These symptoms are known as sciatica.
Patients with degenerative spine conditions commonly report difficulty with everyday activities, as well as lower back pain and symptoms that radiate or shoot down the leg, such as numbness, tingling, or electric shock like symptoms. These symptoms are known as sciatica.










